Abstract
Purpose of Review
Diagnosis of bacterial acute rhinosinusitis is difficult. Several attempts have been made to clarify the diagnostic criteria. Inflammatory biomarkers are easily obtainable variables that could shed light on both the pathophysiology and diagnosis of bacterial acute rhinosinusitis. The purpose of this review article is to assess literature concerning the course of inflammatory biomarkers during acute rhinosinusitis and the use of inflammatory biomarkers in diagnosing bacterial acute rhinosinusitis.
Recent Findings
We included C-reactive protein, erythrocyte sedimentation rate, white blood cell counts, procalcitonin, and nasal nitric oxide in this review and found that especially elevated C-reactive protein and erythrocyte sedimentation rate are related to a higher probability of a bacterial cause of acute rhinosinusitis. Still, normal levels of these two biomarkers are quite common as well, or the levels can be heightened even during viral respiratory infection without suspicion of bacterial involvement.
Summary
Elevated levels of C-reactive protein or erythrocyte sedimentation rate support diagnosis of bacterial acute rhinosinusitis, but due to a lack of sensitivity, they should not be used to screen patients for bacterial acute rhinosinusitis.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl. 2012;23(23):1–298.
Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, et al. Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72–e112. https://doi.org/10.1093/cid/cis370.
Desrosiers M, Evans GA, Keith PK, Wright ED, Kaplan A, Bouchard J, et al. Canadian clinical practice guidelines for acute and chronic rhinosinusitis. J Otolaryngol Head Neck Surg. 2011;40(Suppl 2):S99–193.
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Ashok Kumar K, Kramper M, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1–S39. https://doi.org/10.1177/0194599815572097.
Anon JB, Jacobs MR, Poole MD, Ambrose PG, Benninger MS, Hadley JA, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130(1 Suppl):1–45.
Bachert C, Hörmann K, Mosges R, Rasp G, Riechelmann H, Müller R, et al. An update on the diagnosis and treatment of sinusitis and nasal polyposis. Allergy. 2003;58(3):176–91. https://doi.org/10.1034/j.1398-9995.2003.02172.x.
Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2007 summary. Natl Health Stat Rep. 2010;27(27):1–32.
Berg O, Carenfelt C, Rystedt G, Änggård A. Occurrence of asymptomatic sinusitis in common cold and other acute ENT-infections. Rhinology. 1986;24(3):223–5.
Autio TJ, Tapiainen T, Koskenkorva T, Narkio M, Lappalainen M, Nikkari S, et al. The role of microbes in the pathogenesis of acute rhinosinusitis in young adults. Laryngoscope. 2015;125(1):E1–7. https://doi.org/10.1002/lary.24862.
Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, et al. Rhinosinusitis: developing guidance for clinical trials. J Allergy Clin Immunol. 2006;118(5 Suppl):S17–61. https://doi.org/10.1016/j.jaci.2006.09.005.
Aabenhus R, Jensen JU, Jorgensen KJ, Hrobjartsson A, Bjerrum L. Biomarkers as point-of-care tests to guide prescription of antibiotics in patients with acute respiratory infections in primary care. Cochrane Database Syst Rev. 2014;11:CD010130.
Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999;17(6):1019–25. https://doi.org/10.1016/S0736-4679(99)00135-3.
van der Meer V, Neven AK, van den Broek PJ, Assendelft WJ. Diagnostic value of C reactive protein in infections of the lower respiratory tract: systematic review. BMJ. 2005;331(7507):26–0. https://doi.org/10.1136/bmj.38483.478183.EB.
Whicher JT, Chambers RE, Higginson J, Nashef L, Higgins PG. Acute phase response of serum amyloid A protein and C reactive protein to the common cold and influenza. J Clin Pathol. 1985;38(3):312–6. https://doi.org/10.1136/jcp.38.3.312.
Melbye H, Hvidsten D, Holm A, Nordbø SA, Brox J. The course of C-reactive protein response in untreated upper respiratory tract infection. Br J Gen Pract. 2004;54(506):653–8.
Ruuskanen O, Putto A, Sarkkinen H, Meurman O, Irjala K. C-reactive protein in respiratory virus infections. J Pediatr. 1985;107(1):97–100. https://doi.org/10.1016/S0022-3476(85)80624-7.
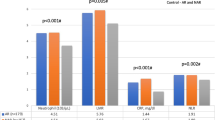
• Autio TJ, Koskenkorva T, Leino TK, Koivunen P, Alho OP. Longitudinal analysis of inflammatory biomarkers during acute rhinosinusitis. Laryngoscope. 2017;127(2):E55–61. Reference 17 is important because the reference standard used in this study for bacterial acute rhinosinusitis was positive bacterial culture from a maxillary sinus aspiration. Therefore, the diagnosis of bacterial acute rhinosinusitis in this study was culture-proven.
• Hansen JG, Højbjerg T, Rosborg J. Symptoms and signs in culture-proven acute maxillary sinusitis in a general practice population. APMIS. 2009;117(10):724–9. Reference 18 is important because the reference standard used in this study for bacterial acute rhinosinusitis was positive bacterial culture from a maxillary sinus aspiration. Therefore, the diagnosis of bacterial acute rhinosinusitis in this study was culture-proven.
• Savolainen S, Jousimies-Somer H, Karjalainen J, Ylikoski J. Do simple laboratory tests help in etiologic diagnosis in acute maxillary sinusitis? Acta Otolaryngol Suppl. 1997;529:144–7. Reference 18 is important because the reference standard used in this study for bacterial acute rhinosinusitis was positive bacterial culture from a maxillary sinus aspiration. Therefore, the diagnosis of bacterial acute rhinosinusitis in this study was culture-proven.
Hansen JG, Schmidt H, Rosborg J, Lund E. Predicting acute maxillary sinusitis in a general practice population. BMJ. 1995;311(6999):233–6. https://doi.org/10.1136/bmj.311.6999.233.
Van Buchem L, Peeters M, Beaumont J, Knottnerus A. Acute maxillary sinusitis in general practice: the relation between clinical picture and objective findings. Eur J Gen Pract. 1995;1(4):155–60. https://doi.org/10.3109/13814789509161629.
Lindbaek M, Hjortdahl P, Johnsen UL. Use of symptoms, signs, and blood tests to diagnose acute sinus infections in primary care: comparison with computed tomography. Fam Med. 1996;28(3):183–8.
Young J, Bucher H, Tschudi P, Periat P, Hugenschmidt C, Welge-Lussen A. The clinical diagnosis of acute bacterial rhinosinusitis in general practice and its therapeutic consequences. J Clin Epidemiol. 2003;56(4):377–84. https://doi.org/10.1016/S0895-4356(02)00590-5.
Autio TJ, Koskenkorva T, Narkio M, Leino TK, Koivunen P, Alho OP. Diagnostic accuracy of history and physical examination in bacterial acute rhinosinusitis. Laryngoscope. 2015;125(7):1541–6. https://doi.org/10.1002/lary.25247.
Hansen JG, Schmidt H, Grinsted P. Randomised, double blind, placebo controlled trial of penicillin V in the treatment of acute maxillary sinusitis in adults in general practice. Scand J Prim Health Care. 2000;18(1):44–7.
Kratz A, Plebani M, Peng M, Lee YK, McCafferty R, Machin SJ, et al. ICSH recommendations for modified and alternate methods measuring the erythrocyte sedimentation rate. Int J Lab Hematol. 2017;39(5):448–57.
Brigden ML. Clinical utility of the erythrocyte sedimentation rate. Am Fam Physician. 1999;60(5):1443–50.
Puhakka T, Mäkelä MJ, Alanen A, Kallio T, Korsoff L, Arstila P, et al. Sinusitis in the common cold. J Allergy Clin Immunol. 1998;102(3):403–8. https://doi.org/10.1016/S0091-6749(98)70127-7.
Werman HA, Brown CG. White blood cell count and differential count. Emerg Med Clin North Am. 1986;4(1):41–58.
Stock W, Hoffman R. White blood cells 1: non-malignant disorders. Lancet. 2000;355(9212):1351–7. https://doi.org/10.1016/S0140-6736(00)02125-5.
McClain MT, Park LP, Nicholson B, Veldman T, Zaas AK, Turner R, et al. Longitudinal analysis of leukocyte differentials in peripheral blood of patients with acute respiratory viral infections. J Clin Virol. 2013;58(4):689–95. https://doi.org/10.1016/j.jcv.2013.09.015.
Davies J. Procalcitonin. J Clin Pathol. 2015;68(9):675–9. https://doi.org/10.1136/jclinpath-2014-202807.
Gilbert DN. Procalcitonin as a biomarker in respiratory tract infection. Clin Infect Dis. 2011;52(Suppl 4):S346–50. https://doi.org/10.1093/cid/cir050.
Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004;39(2):206–17. https://doi.org/10.1086/421997.
Djupesland PG, Chatkin JM, Qian W, Haight JS. Nitric oxide in the nasal airway: a new dimension in otorhinolaryngology. Am J Otolaryngol. 2001;22(1):19–32. https://doi.org/10.1053/ajot.2001.20700.
Scadding G, Scadding GK. Update on the use of nitric oxide as a noninvasive measure of airways inflammation. Rhinology. 2009;47(2):115–20.
Lanz MJ, Prendes S, Peyrou N, Toledo G, Ferrer CM. Nasal nitric oxide as a noninvasive marker in the antibiotic treatment of acute bacterial sinusitis. J Allergy Clin Immunol. 2008;121(2):530–1. https://doi.org/10.1016/j.jaci.2007.09.034.
Baraldi E, Azzolin NM, Biban P, Zacchello F. Effect of antibiotic therapy on nasal nitric oxide concentration in children with acute sinusitis. Am J Respir Crit Care Med. 1997;155(5):1680–3. https://doi.org/10.1164/ajrccm.155.5.9154876.
de Winter-de Groot KM, van der Ent CK. Measurement of nasal nitric oxide: evaluation of six different sampling methods. Eur J Clin Investig. 2009;39(1):72–7. https://doi.org/10.1111/j.1365-2362.2008.02064.x.
American Thoracic Society & European Respiratory Society. ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med. 2005;171(8):912–30.
Repka-Ramirez S, Naranch K, Park YJ, Clauw D, Baraniuk JN. Cytokines in nasal lavage fluids from acute sinusitis, allergic rhinitis, and chronic fatigue syndrome subjects. Allergy Asthma Proc. 2002;23(3):185–90.
Rudack C, Stoll W, Bachert C. Cytokines in nasal polyposis, acute and chronic sinusitis. Am J Rhinol. 1998;12(6):383–8. https://doi.org/10.2500/105065898780708008.
Riechelmann H, Deutschle T, Rozsasi A, Keck T, Polzehl D, Burner H. Nasal biomarker profiles in acute and chronic rhinosinusitis. Clin Exp Allergy. 2005;35(9):1186–91. https://doi.org/10.1111/j.1365-2222.2005.02316.x.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Rhinosinusitis
Rights and permissions
About this article
Cite this article
Autio, T.J., Koskenkorva, T., Koivunen, P. et al. Inflammatory Biomarkers During Bacterial Acute Rhinosinusitis. Curr Allergy Asthma Rep 18, 13 (2018). https://doi.org/10.1007/s11882-018-0761-2
Published:
DOI: https://doi.org/10.1007/s11882-018-0761-2